How to use eConsent Efficiently in Medical Device Studies

Medical device manufacturers rely on clinical trials and research studies to ensure their devices get approved for mainstream use. Clinical trial managers have to be very careful about gaining the consent of participants, recording that consent, and ensuring patients are informed of any changes that could affect their willingness to participate.
The COVID-19 pandemic drove the increased use of eConsent, and taught us all the importance of considering remote alternatives. Therefore it is important that medical device companies know how to use electronic consent modules efficiently, effectively, and with patients’ experience in mind.
What is eConsent in Clinical Trials?
eConsent (electronic consent) means simply giving consent to participate in research activities, such as clinical trials, electronically. It’s a digital replacement for a traditional “wet” or ink signature.
In one of our recent webinars, a poll showed that most participants had not used eConsent before. However, many were familiar with at least the concept of eConsent. There has certainly been recent accelerated use of eConsent in direct-to-patient (DTP) studies and decentralized clinical trials (DCTs). Clinical trial managers may find that gathering information digitally is safer, and simpler, than handing in documents face-to-face or sending them through the post. However, not all eConsent is done remotely.
Why eConsent in Clinical Trials?
Some of the advantages to using eConsent are:
- Electronic storage & back-up
- 2-step authentication
- Documentation of necessary privacy law confirmations
- Consent version control
- Reduced in-person monitoring
With electronic signatures, medical device manufacturers can store, and back up respondents’ data electronically. This gives administrators ease of access to individual records, or an overview of everyone who participates in a particular study. Two-step authentication provides a high level of security for this data.
Electronic data capture tools also allow study participants to be shown necessary privacy law requirements, such as the GDPR, and keep a record that they confirmed they’re aware of their rights.
Finally, one last consideration for digital consent is that it reduces the requirement for in-person monitoring. However, even face-to-face consent that allows participants to engage with investigators brings all the advantages highlighted above.
Key considerations for implementation
Consent may fall under ISO 14155:2020 and ISO 20916:2019, which cover good clinical practice and good study practice relating to medical devices for human subjects. These documents comprise the fact that participants in studies must give informed consent. ISO 14155:2020 section 3.27 describes informed consent as:
“[The] process by which an individual voluntarily confirms willingness to participate in a particular clinical investigation, after having been informed of all aspects of the investigation that are relevant to the decision to participate.”
This is key for all clinical studies, there are no shortcuts with consent, and there shouldn’t be. Implementing eConsent requires that these guidelines are taken into account, providing potential participants with every bit of information they need in order to make an informed decision.
Any eConsent module should also encourage adherence to the principles of informed consent, such as not allowing participants to continue if they haven’t reviewed the relevant information. Too many apps permit users to skip past the Terms & Conditions (T&Cs). eConsent cannot allow this and remain fit-for-purpose.
What are the key considerations to effectively unlock the efficiencies of eConsent?
The following are several key considerations that support medical device companies in using eConsent efficiently.
- Study site or location - different locations have distinctive guidelines around eConsent. When considering the use of eConsent, it is pivotal to check local regulations and guidelines and verify if eConsent is feasible in that specific location.
- In-person consenting is always preferable - also when using eConsent - because it allows the participant to ask the investigator any questions.
- The right technology - ensure web-based access to make consent available to patients without digital devices.
- Setup and test with actual users - ideally, set up a test as close to the real process as possible to follow the flow and make sure everything works.
- No study too big or too small - great eConsent modules should work well for any size study.
Clinical investigation - use case #1
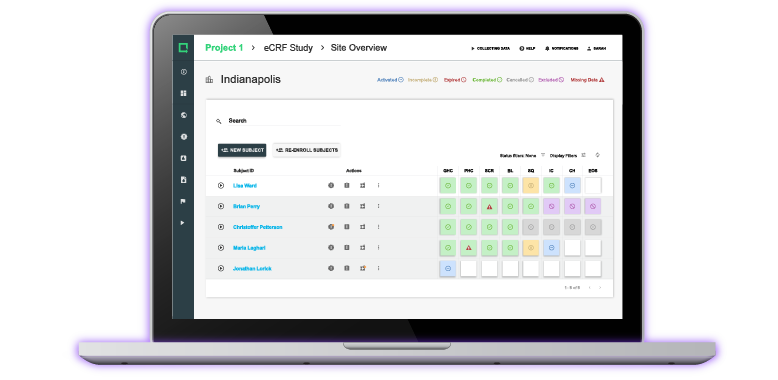
The first use case we’re looking at is for an implantable device, where a participant would visit the physician’s office. It is assumed they use Greenlight Guru Clinical (formerly SMART-TRIAL) with the eConsent module. The details of this case are as follows:
- Class III implantable device
- Study across 15 sites spanning Europe and the United States
- One year study with a five-year follow-up
- 200 patients, mostly from older age groups
- Mid-study protocol change
- Greenlight Guru Clinical used with eConsent module
The significance of the participants’ age is that many of them could be less comfortable with the technology required for digital consent. They have to visit the site, but they may not own devices or bring any with them. Therefore, the site must provide web-based access for patients where necessary.
The other important factor is the mid-study protocol change. ISO 14155:2020 section 5.8.2 (j) specifically states, as part of the consenting process, to ‘’ensure important new information is provided to new and existing subjects throughout the clinical investigation, which may relate to the subject’s willingness to continue participation in the clinical investigation.
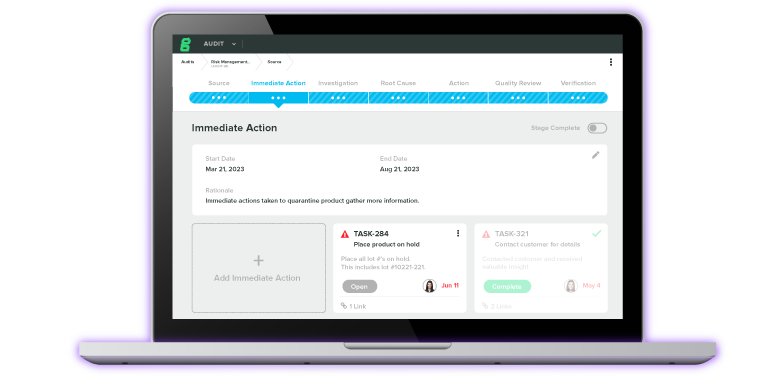
In other words, participants must be given information regarding any changes as well as the option to opt out of further participation. Greenlight Guru Clinical offers the functionality to update and inform participants within an hour or less.
Greenlight Guru Clinical (formerly SMART-TRIAL) provides various efficiencies in this use case, including:
- Digitally recorded consent
- Consent procedures handled entirely by Greenlight Guru Clinical
- Consent is easily monitored by team members conducting a central review
- Re-consenting is made simple for patients affected by mid-study protocol change
- Quick, easy, and secure for patients, plus it protects their privacy by blanking out certain details such as their email address
The advantages over paper consent forms are clear and go far beyond the obvious storage and environmental factors of storing hundreds of sheets of paper securely.
Registries and retrospective - use case #2
The next use case consists of a much larger group, with more complex factors. The key points for this study are:
- Class III implantable device
- 100 sites in Europe and the United States
- Device CE marked in 2018
- Expecting FDA PMA Q2/2023
- 1,600 patients, again from older age groups
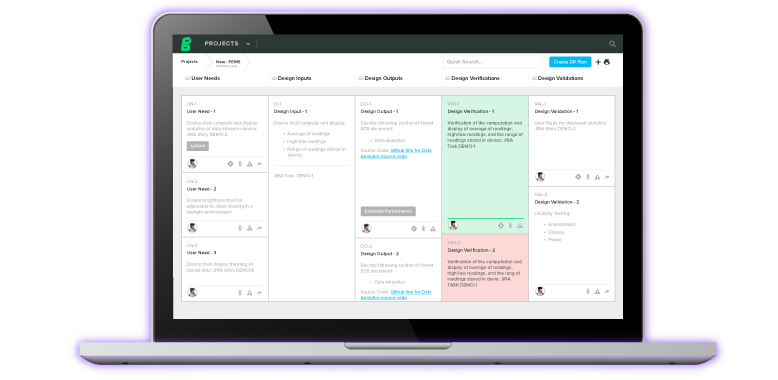
- Greenlight Guru's EDC system used
In this case, a renewal of the CE marking is required, meaning additional evidence is needed. The American study won’t conclude until after the CE marking submission is made, and it’s not possible to simply remove the device from the European market. So, there’s a huge volume of data available from users in Europe, but they’ve not given consent to provide their data as evidence.
Greenlight Guru Clinical can in this case be used to set up a registry database and request consent from existing and new patients. That consent can then be monitored by a central review team. The same registry works for existing patients (patients from the American study), and any new patients or study participants to keep the data as useful as possible. This really speeds up the process for medical device manufacturers without the losses of taking a device off the market.
Greenlight Guru Clinical Streamlines Clinical Data Collection
Clinical trial managers and medical device manufacturers need simpler processes that take the patient experience into account without cutting corners. Find out more about how Greenlight Guru Clinical’s services can empower you to do just that.
Páll Jóhannesson, M.Sc. in Medical Market Access, is the founder and Managing Director of Greenlight Guru Clinical (formerly SMART-TRIAL). Páll was previously the CEO of Greenlight Guru Clinical where he led the team to create the only EDC specifically made for medical devices.